
Credentialing & Recertification
Our team of specialists at CDWT maintains expertise in the provider credentialing process, keeping current of industry developments, credentialing trends, and payer needs. As specialists, we handle the whole credentialing procedure. This implies that our team assumes all of the obligations that would normally fall to your personnel, allowing them to concentrate on more crucial activities.
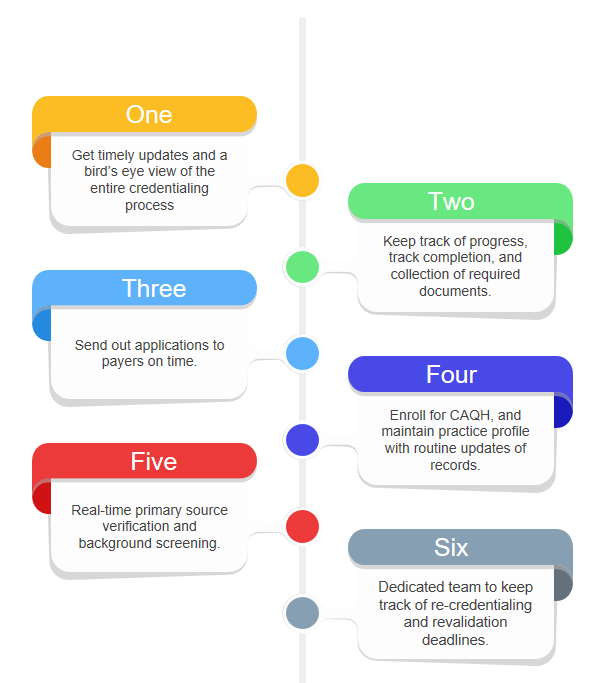
We monitor the completion and collection of all required papers, complete the credentialing process, submit applications to payers, and promptly reply to any requests from payers for adjustments or further information. Each time your practise is due for re-credentialing, CDWT assigns a team of experts to monitor re-credentialing dates, commence the process, and finish it.
Our staff collaborates with the provider to complete the first application, undertake organization-required duties such as primary source verification and background screening, and communicate with payers to facilitate prompt approval and speed provider starts.
Facilitate Your Practice's Prosperity
Trust the specialists at CDWT to guide you through the complex process of provider enrollment and medical credentialing at an affordable price! No more cash flow issues and nonpayment. No more data mistakes. No more unintentional expirations; we'll put a stop to all of your problems. Contact us immediately.
Here are Our Services:
Data Gathering
CAQH Enrollment
Offer Applications
Active Interaction
Completely Open Access
Customer Service Representative
Certification is a Crucial Component
Provider credentialing is a fundamental responsibility since practises that provide unbillable treatments are neither realistic nor sustainable for a medical organization.
The credentialing process guarantees that the provider satisfies the requirements of the medical organisation and its payers, as well as identifies risk indicators early on to limit the likelihood of unfavourable consequences. In addition, credentialing is an excellent technique to boost public relations in order to attract new patients and earn their confidence.
Credentialing is time-consuming, but it protects your income, reduces the danger of possible loss, and increases the reputation of your practise.
Medicare
Medicaid
BCBS
Aetna
Humana
Health Partners
Cigna Health
We'll Take Care of the Paperwork
Numerous practitioners attempt to handle the medical provider certification process internally. However, after analyzing the costs, the majority have determined that outsourcing to CDWT is the most cost-effective option.
When you outsource your credentialing to a team of specialists, your efforts may be consolidated; while your staff may be certifying one or two (or even twenty) providers at a time, CDWT’s team is capable of credentialing dozens of providers simultaneously, every day. This not only saves you money, but also frees up your staff’s precious time to concentrate on other vital tasks, so assuring the development of your practice.
Permit our Credentialing Service to handle the credentialing and continuous maintenance of providers. Our specialists are familiar with all payers, their requirements, and the necessary steps to get credentialing. CDWT delivers comprehensive transparency and monthly updates throughout the payer credentialing process.






